Innovation
Endurance training:
Resistance training is a component essential training for patients with ILD and most studies have included it People with ILD may need more careful planning and modification of their exercise prescription than healthy people or those with COPD, due to the severity of dyspnea due to exertion, profound exercise-induced oxyhemoglobin desaturation, and rapid progression of the disease in some patients.
Resistance training aims to improve aerobic capacity, increase exercise endurance, and improve daily function and physical activity with reduced shortness of breath and fatigue.
The initial intensity of resistance training
It is generally set between 70 and 80% of the maximum exercise capacity. A minimum frequency of two sessions supervised by a doctor is suggested.The target duration of resistance exercise in each session should be 30 minutes, divided into shorter intervals if necessary (for example, 15 minutes on a stationary bike and 15 minutes of walk, either on a treadmill or on a runner). Most participants achieve this duration of exercise within 1 to 2 weeks of training, with the proper support of an experienced doctor.
Participants should be encouraged to assess their dyspnea and fatigue regularly during exercise. Also intermittent monitoring of the saturation and heart rate. Once I know it reaches a duration of 30 minutes, the progression produced by regular increases in exercise intensity (e.g. weekly increase in walking speed or cycling work rate). It should also be recommended to participants adopt a home exercise program, aiming to complete 3-5 resistance exercise sessions each week.
Interval training
Interval training can provide an alternative exercise modality to training of resistance in EPID. Interval training consists of periods of relatively high-speed exercise.intensity interspersed with periods of low intensity exercise with or without rest. The objective of interval training is to allow patients to achieve the required training dose through repeated sets rather than continuous exercise, which may reduce breathlessness and fatigue. The ATS/ERS statement for RR suggests that interval training can be performed with less symptoms than continuous training. Regarding DILD, few published studies included interval training, although several are currently underway. The authors of a systematic review of interval training in COPD reported a variety of interval training regimens in this group, including: two studies with intervals of 1 minute of higher intensity [>90% of maximum power (Ppeak)], alternating with 2 minutes of low intensity (<75% of peak); three trials with 30 second intervals (100/45% peak); a study with high (50% peak) and low (10% peak) intervals of 20 and 40 seconds; and a 2 minute high intensity interval study (90% peak) and 1 minute of low intensity (50% peak). There were no significant differences in exercise capacity and HRQoL between interval training and continuous training. More study of interval training is required in ILD.
Evaluation System
This literature review includes clinical trials with patient data, so it implies a qualitative analysis of the data.
Assessment
This literature review includes clinical trials with patient data, so it implies a qualitative analysis of the data.
References
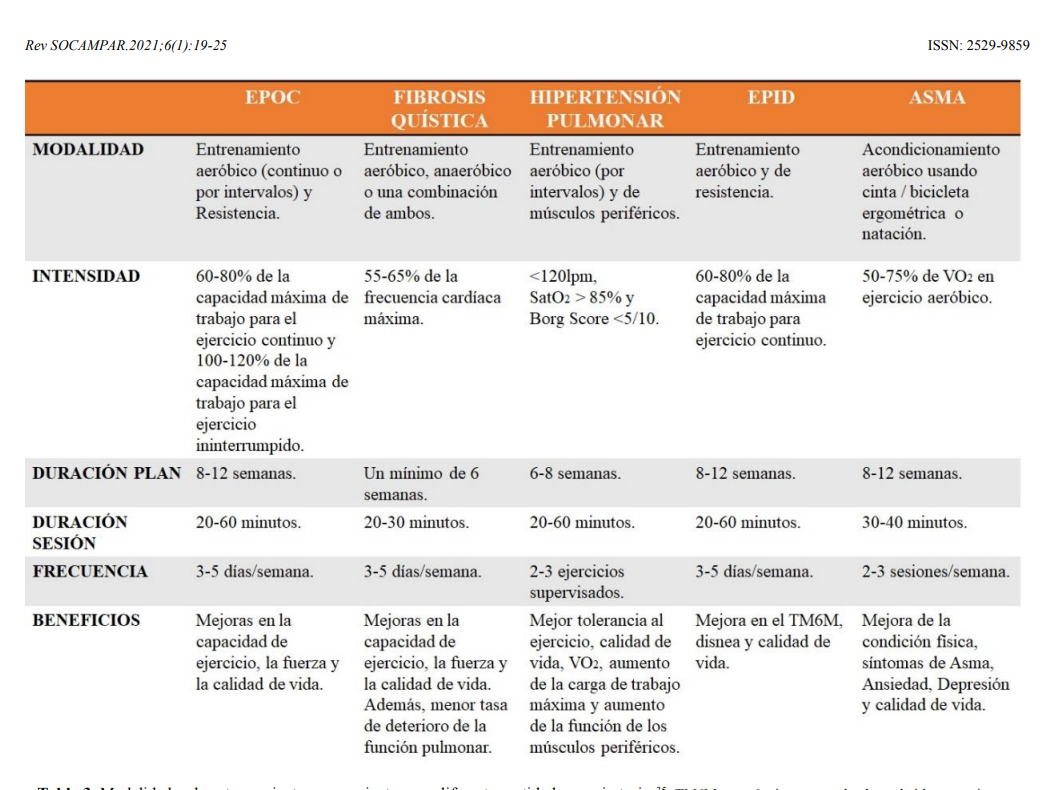
A systematic review: benefits of physical exercise in diffuse interstitial lung disease. Bonmatí; Hurtado Fuentes; Sánchez Villar; Alcaraz Barcelona; García Castillo; Cruz Ruiz; Genovés Crespo; Godoy Mayoral; Callejas González. Rev SOCAMPAR.2021;6(1):19-25.ISSN: 2529-9859